Local anesthesia is a cornerstone of modern dentistry, ensuring that patients can undergo dental procedures with no pain and discomfort. However, despite its widespread use and effectiveness, local anesthesia can sometimes fail, leading to patient distress and complicating dental treatments. The failure of local anesthesia in dentistry can be attributed to several factors, like anatomical variations, technical errors, pharmacological issues, and patient-related factors.
Anatomical Variations
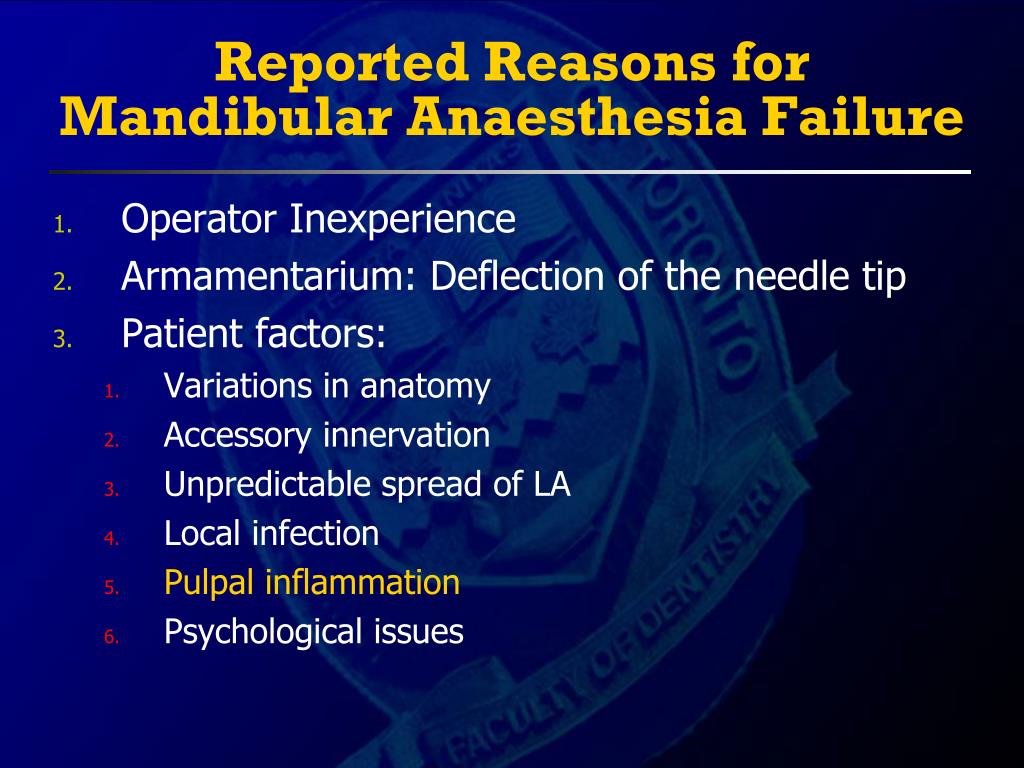
One of the primary reasons for the failure of local anesthetic techniques is the complex and variable orofacial anatomical variations. The success of local anesthesia depends on the precise deposition of the anesthetic solution near the target nerve anatomy. However, anatomical variations can make it difficult to achieve effective anesthesia. The anatomical variations include;
Bone density variations: Unusual bone density in the orofacial region can impede the diffusion of anesthetic solutions, reducing their effectiveness in blocking nerve signals.
Mandibular foramen variability: In some patients, position of mandibular foramen makes it highly challenging to block the Inferior Alveolar nerve effectively. This nerve is responsible for sensation in the lower teeth.
Accessory innervation challenges: An accessory nerve that is not anesthetized can still transmit pain signals, leading to failure of local anesthesia.
Dentist’s Expertise
The expertise of a dentist plays a crucial role in the success of local anesthesia in dentistry. Precise knowledge of orofacial anatomy, proper technique, and the ability to adapt to anatomical variations are essential for achieving effective anesthesia. A skilled dentist can accurately locate the target nerve, select the appropriate anesthetic agent, and use the correct injection technique to maximize the likelihood of success. Factors such as needle angulation, depth of insertion, and aspiration to avoid intravascular injection require clinical proficiency and experience. Additionally, a dentist’s ability to recognize and manage anesthetic failures—whether due to anatomical variations, accessory innervation, or pathological conditions—ensures patient comfort and procedural efficiency. Thus, the success of local anesthesia is not solely dependent on the anesthetic agent but also on the dentist’s expertise and technique.
Pharmacological Factors
The pharmacological properties of the local anesthetic agent itself can also contribute to failure. Factors such as the concentration of the anesthetic, its pH, and the presence of vasoconstrictors can influence its efficacy. In some cases, the anesthetic may not have sufficient potency to block nerve conduction effectively, especially in areas with dense innervation or high pain sensitivity. The pH of the anesthetic solution affects its ability to penetrate nerve tissues. If the solution is too acidic, it may not diffuse well into the nerve, leading to incomplete anesthesia. The use of vasoconstrictors, such as epinephrine, prolong the duration of anesthesia, but if not used appropriately, it can also reduce the effectiveness of the anesthetic by limiting its spread.
Patient-Related Factors
Patient-related factors can also play a significant role in the failure of local anesthesia. Anxiety and fear are common among dental patients, and these emotions can heighten pain perception. These heightened perceptions make patients believe anesthesia has failed. Some patients may have a higher pain threshold or increased sensitivity to pain, requiring a larger dose or a different type of anesthetic. Certain medical conditions, such as infections or inflammation at the injection site, can also reduce the effectiveness of local anesthesia. An abscess alters the pH of the tissue, making it more difficult for the anesthetic to work. Moreover, patients who are chronic users of certain medications, such as opioids or alcohol, may develop a tolerance to local anesthetics, requiring higher doses for effective pain control.
In rare cases, some patients exhibit a natural tolerance or resistance to local anesthetics. This can be due to genetic factors that affect the way their body metabolizes the anesthetic agent. Certain genetic mutations can lead to increased activity of enzymes that break down local anesthetics, reducing their effectiveness. In such cases, the dentist may need to use a different type of anesthetic or adjust the dosage to achieve the desired effect.
Psychological Factors
Psychological factors, such as dental phobia or previous traumatic dental experiences, can significantly impact the perception of pain and the effectiveness of local anesthesia. Patients who are highly anxious or fearful may interpret even minor discomfort as pain, leading them to believe that the anesthesia has failed. In such cases, the dentist may need to employ additional strategies, such as sedation or behavioral techniques, to help the patient relax and improve the overall experience.
Inflammation and Infection
In cases where there is acute inflammation or infection at the site of the dental procedure, local anesthesia may be less effective. Inflammatory processes can alter the local tissue environment, making it more difficult for the anesthetic to penetrate and block nerve conduction. For example, in cases of pulpitis (inflammation of the dental pulp), the acidic environment created by the infection can reduce the efficacy of the anesthetic. In such situations, dentists may need to use alternative techniques, such as intraligamentary or intraosseous anesthesia, to achieve adequate pain control.